

Carol Duff MSN, BA, RN
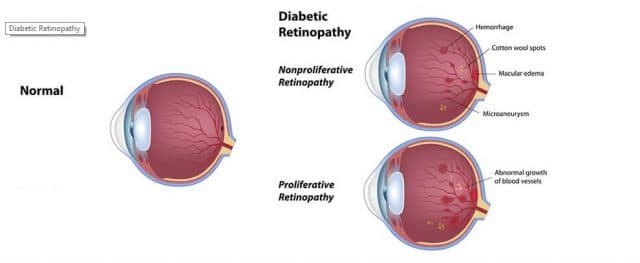
Diabetic retinopathy (DR) affects the eye and is a diabetes complication. Damage to the eyes occurs when the retina, which is the layer of cells which lays at the back of the eye, develops injury to the blood vessels that supply it with oxygenated blood. The retina is sensitive to light and triggers nerve impulses which pass through the optic nerve to the brain where these impulses are interpreted in the form of a visual image. If the blood supply to this very important area of the brain is altered, the retina will suffer from lack of an oxygen supply and not be able to do its job.
Diabetic neuropathy can develop from uncontrolled blood sugar levels in either Type 1 or Type 2 diabetes as well as gestational diabetes. This disease will affect both eyes and may begin with no symptoms. Some symptoms may be:
- Floaters (spots of dark strings floating/suspended in your vision.
- Impaired color vision.
- Vision changes.
- Altered color vision.
- Empty or dark areas in your field of vision.
- Seeing rings around lights.
- Flashing lights.
- Actual loss of vision.

Having high levels of uncontrolled sugar in your blood can/will cause a blockage of the tiny blood vessels that bring oxygen to the retina. When the retina does not receive enough oxygen, the body will try to remedy this issue by producing new blood vessels which do not develop properly and may leak. People with untreated diabetes have a 25 per cent higher risk for blindness.
There are four types/progressive levels of diabetic retinopathy:
Early/mild diabetic retinopathy (nonproliferative diabetic retinopathy (NPDR). Nonproliferative means that new blood vessels are not growing or proliferating. This type of retinopathy is the most common form with the walls of the blood vessels in the retina becoming weak. There may be microaneurysms (tiny bulges in the walls of the blood vessels) which will leak blood and fluid into the retina. While this is occurring, the larger blood vessels may begin to dilate. As more blood vessels are involved and become blocked, NPDR progresses from mild to severe. In addition, nerve fibers of the retina may start to swell. If the macula (central part of the retina) begins to swell, macular edema will develop and will require treatment.
Moderate nonproliferative retinopathy. In the progression of this disease blood vessels to the retina may swell and twist and lose the ability to transport oxygenated blood.
Severe nonproliferative retinopathy. Additional blood vessels are blocked and growth factors to stimulate the production of new blood vessels are produced. The growth factors will produce inadequate blood vessels.
Advanced Proliferative Diabetic Retinopathy (PDR) is a progression to proliferative diabetic retinopathy (PDR). The damaged blood vessels close off and this causes the growth of new, abnormal blood vessels in the retina. These new vessels can leak into the vitreous humor (clear, jelly-like substance which fills the main portion of the eyeball.) Ultimately, the scar tissue caused by this new growth of blood vessels may cause the retina to detach from the back of the eye. New vessels may also interfere with the normal flow of fluid out of the eyeball and cause an increase in pressure in the eye, called glaucoma (see Glaucoma, the Unseen Enemy on VT web site). The retina may peel away from the back wall of the eye leading to a retinal detachment that can cause permanent loss of vision. PDR can take away both peripheral (your vision to the side of your visual field) and central vision.
 Anyone who has diabetes (Type 1, Type 2, and Gestational) has a chance of developing diabetic retinopathy. Other risk factors can be involved and these factors are:
Anyone who has diabetes (Type 1, Type 2, and Gestational) has a chance of developing diabetic retinopathy. Other risk factors can be involved and these factors are:
- Poor control of blood sugar levels.
- The longer you have diabetes the more likely you will develop the above changes to the eye.
- High blood pressure.
- High cholesterol.
- Use of tobacco.
- Being Hispanic, Native American, or those of African/Sub Saharan descent.

Testing for diabetic retinopathy will include an ophthalmologist putting drops into your eyes to widen the pupil (black center part) so the inside of your eye may be viewed with a special lens. A visual acuity test using the eye chart test for your distance vision will also be performed. Tonometry, which is a test to measure the inside pressure of your eye, is also part of the exam. You doctor may also do fluorescein angiography to see how your retina is affected. Dye will be injected into a vein in your arm and will move through the blood vessels. A specialized camera will take photos of the retina as the dye moves through your blood stream. The results of this test will show if you have any blocked, leaking, or any abnormal blood vessels.

Another test may be an optical coherence tomography (OCT). Diabetic macular edema (DME), or swelling of the macula, may go along with retinopathy. A machine takes images of the retina and gives thickness of this portion of the eye, which helps the doctor to find and measure swelling of the macula of each eye.

Prevention of DR:
- Early detection and treatment will reduce the risk of blindness by 95%.
- Receive a comprehensive dilated eye exam at least once a year. People who are already diagnosed with DR need will need more frequent eye exams.
- Pregnant women who have diabetes should have a comprehensive eye exam as early in the pregnancy as possible. Additional exams during the pregnancy may be necessary.
- Keep blood sugar levels as close to normal as possible.
- Controlling blood pressure and cholesterol may reduce the risk of vision loss in diabetics.

Treatment for DR is based on the physical exam of your eyes and may include:
- Medical control with measures (diet, exercise, insulin, regular blood sugar level testing) used to regulate your blood sugar levels and decrease high blood pressure. Sometimes adhering to all the basics to control blood sugar levels can return some of your lost vision.
- Medicines, of which one type is called “anti-VEGF” medication may be prescribed to decrease the swelling of the macula and slow the loss of or improve vision. This type of drug is given by injections into the eye. Some anti-VEGF drugs are Avastin (bevacizumab), Lucentis (ranibizumab), and Eylea (aflibercept). Lucentis and Eylea are approved by the U.S. Food and Drug Administration (FDA) for treating DME. Avastin was approved by the FDA to treat cancer, but is commonly used to treat eye conditions, including DME. Typically, there may be monthly anti-VEGF injections for the first six months of treatment. After six months, there will be three to four injections for the second six months of treatment, four in the second year of treatment, two injections in the third year, one in the fourth year and none in the fifth year.
- Corticosteroids may be injected or implanted into the eye and can be used alone or in a combination with other drugs or laser surgery to treat DME. The risk of cataracts and glaucoma are increased with corticosteroid use. DME patients who use corticosteroids should be monitored for increased pressure in the eye and glaucoma. The type of medications you receive will be determined by your doctor.
- Laser surgery may be used to seal off leaking blood vessels and to help shrink blood vessels which both cause swelling of the retina. Scatter laser surgery (panretinal laser surgery or panretinal photocoagulation) treatment involves making 1,000 to 2,000 tiny laser burns in areas of the retina, excluding the area of the macula. The laser surgery is projected to cause the abnormal blood vessels to shrink. Although treatment can be completed in one session, two or more sessions are sometimes required. This treatment may cause some loss of peripheral, color, and night vision. Scatter laser surgery works best before new blood vessels have started to bleed.
- A vitrectomy (removal of vitreous gel, scar tissue, and/or blood from leaking vessels in the eye) will allow more light rays to penetrate the vitreous humor in the main section of the eye and focus on the retina.
References:
American Academy of Ophthalmology www.aao.org
American Society of Retina Specialists www.asrs.org
Kellogg Eye Center Michigan Medicine www.umkelloggeye.org
Mayo Clinic www.mayoclinic.org/diseases
National Eye Institute (NIH) www.nei.nih.gov

Carol graduated from Riverside White Cross School of Nursing in Columbus, Ohio and received her diploma as a registered nurse. She attended Bowling Green State University where she received a Bachelor of Arts Degree in History and Literature. She attended the University of Toledo, College of Nursing, and received a Master’s of Nursing Science Degree as an Educator.
She has traveled extensively, is a photographer, and writes on medical issues. Carol has three children RJ, Katherine, and Stephen – one daughter-in-law; Katie – two granddaughters; Isabella Marianna and Zoe Olivia – and one grandson, Alexander Paul. She also shares her life with her husband Gordon Duff, many cats, and two rescues.
ATTENTION READERS
We See The World From All Sides and Want YOU To Be Fully InformedIn fact, intentional disinformation is a disgraceful scourge in media today. So to assuage any possible errant incorrect information posted herein, we strongly encourage you to seek corroboration from other non-VT sources before forming an educated opinion.
About VT - Policies & Disclosures - Comment Policy




Comments are closed.